Multidrug-Resistant Klebsiella pneumoniae from Pediatric Sepsis Patients in Nigeria
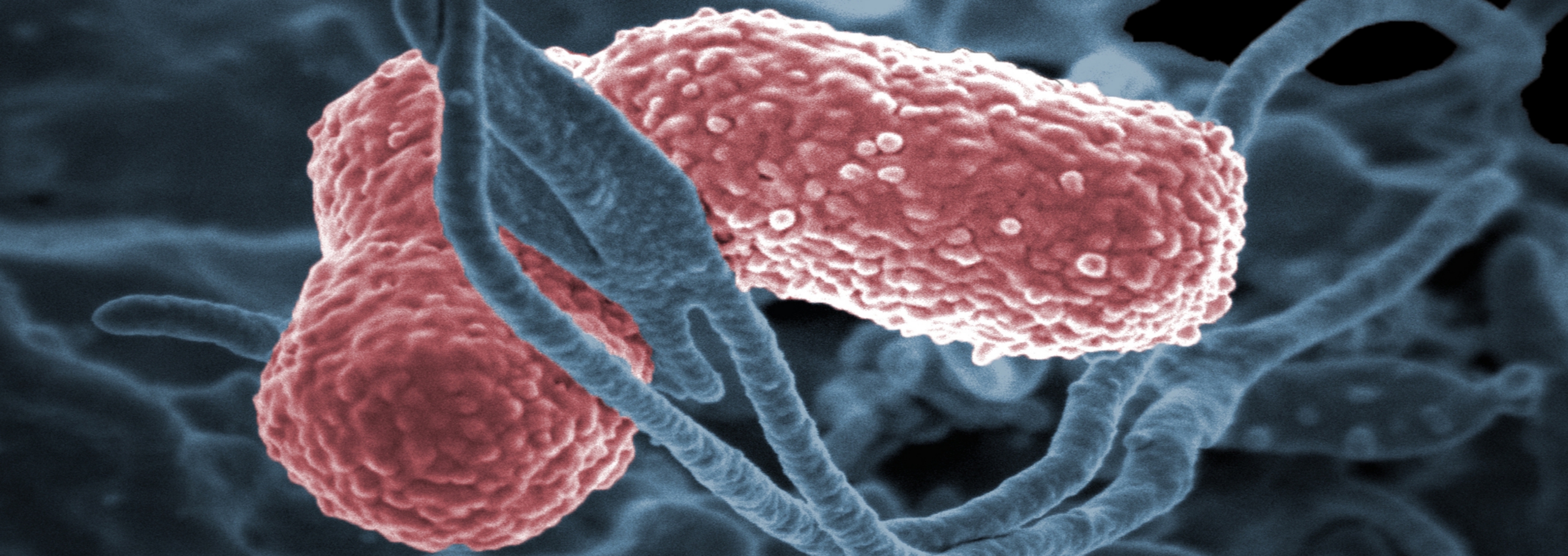
Although the role of invasive bacterial infections has been recently acknowledged as a leading cause of mortality in several African countries, debate is ongoing as to the characteristics of these agents, largely in part due to the absence of functional microbiology diagnostic services. Dr. Stephen Obaro recently established microbiology diagnostic laboratories at two regional locations in central Nigeria and have demonstrated the role of multidrug resistant Enterobacteriaceae, particularly Klebsiella pneumoniae, in morbidity and mortality in young children with bacteremia. In 2013, Dr. Obaro established an additional surveillance site in Kano, northwest Nigeria. Between September 2008 and April 2015, at both locations in Abuja, including a number of suburban settlements and Kano metropolis, 10,133 children were screened. Clinically significant bacteremia was detected in 609 of 4,051 (15%) in Kano and 457 of 6,082 (7.5%) in Abuja. Klebsiella spp is the third leading cause of deaths with a case fatality rate of 20%. In infants, however, the leading cause of bacteremic deaths is Klebsiella spp with a case fatality rate of 19.4%. During the month of April 2016, there was an outbreak of K. pneumoniae sepsis in the newborn unit of one of teaching hospitals. There 54 in-patients and while only about 22 of these had a blood culture drawn, there were 9 babies with confirmed K. pneumoniae bacteremia and 4 of these died. There exists little knowledge of strain diversity and AMR resistance mechanisms in this Nigerian cohort.
Genomes of 75 isolates will be sequenced in a bar-coded paired-end library for 2x150 bp paired end reads on the Illumina NextSeq 500 and annotated by NCBI. The genomes of all sequenced strains, including the other currently available K. pneumoniae genomes, will be used to compare multiple genomes as the Pangenome of the species using PanOCT. The results include tables of core genes, shared genes and strain specific genes, along with role category and GO term enrichment of each type of gene. A phylogeny will be constructed based on gene presence/absence and based on SNPs in core genes (using NASP). We will compare the gene repertoire of strains that were colonizers vs causing invasive infection.
Funding
This project has been funded in whole or part with federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services under Award Number U19AI110819.